Medicaid providers who have not billed for services in more than a year will be disenrolled form the state’s Medicaid program, DHS officials announced today. This effort is aimed at eliminating a portion of the state’s skyrocketing Medicaid fraud problem. On October 15th around 800 providers were disenrolled. These providers have not billed for their services since April 1, 2024.
This is welcome news. It seems odd to be enrolled as an eligible provider without billing in over 18 months, so if you do not routinely provide that service, you should have to re-enroll to be a provider who can bill the state. However, the same should be doubly true for their patients. If you have no contact with a doctor or insurer for your Medicaid for years, someone should at minimum hear from you.
But after years of automatically reenrolling people on Medicaid whether or not they want to continue to be on Medicaid, the state needs to wake up. If someone is on Medicaid in Minnesota, their bills are largely paid by an insurance company who covers them on behalf of the state. That company is paid by the state with a mix of state and federal dollars. Many of those enrollees do not know they are on Medicaid.
According to the report “What the Medicaid undercount reveals about Medicaid Unwinding” completed last year by the Center of the American Experiment, as many as one-in-five enrollees in Medicaid are having their enrollment paid for by taxpayers despite them being in another state,on another plan or dead. This number jumped from 5.8 million in 2019 to 18.5 million in 2022.
This spike corresponds with covid-era legislation to load people onto public programs and prohibit their disenrollment. The Paragon Institute found an even greater spike in “phantom policies” in the individual Obamacare market. Paragon’s research found a jump of 15% of patients who had no contact with a doctor over the past year, while the numbers in the small group market remained steady over the same time period. This indicates most of these new plans in the individual market are “phantom policies” with no real patient.
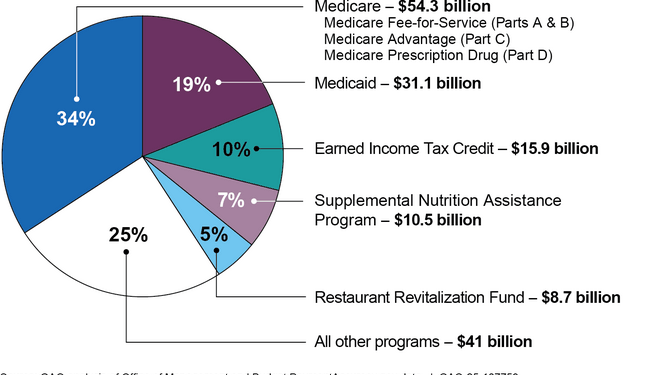
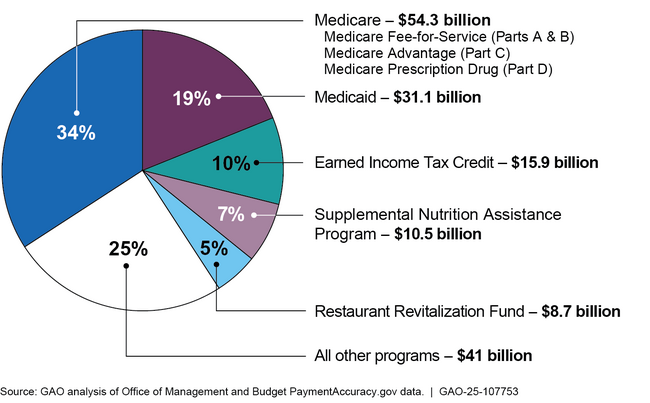
The Big Beautiful Bill (O3B) provides for more routine redetermination to make sure ineligible enrollees are disenrolled. The General Accounting Office outlines $85 billion in improper payments in Medicaid and Medicare in 2024.
IMPROPER PAYMENTS 2024
If someone is ineligible because they live in another state, are on another program, or are dead, the taxpayers should stop paying the insurance companies for their care. Legislation to withhold a portion of the payments to insurance companies until they find that a patient is alive, lives in the state and wants Medicaid (I’m Not a Robot Bill”) passed the House Health committee last year but then died. Hopefully this will get traction next year.
Minnesota can no longer afford to pay fake providers or phantom patients. “We must reduce risk and increase efficiencies wherever we can,” said Temporary Human Services Commissioner Shireen Gandhi. Amen, Ms Gandhi. Now is the time to start really reducing improper payments.